
The Leading Non-Surgical Knee Pain Treatment in Houston: Effective Relief Without Surgery
Knee pain can derail daily life, limit work and exercise, and make basic tasks like climbing stairs painful; non-surgical knee pain treatment offers effective, lower-risk alternatives that focus on healing and function rather than immediate joint replacement. This article explains what non-surgical options are available in Houston, how they work biologically, which knee conditions respond best, and how to choose a personalized pathway that aims to avoid drugs and surgery when appropriate. Readers will learn common causes such as osteoarthritis and meniscal injury, the mechanisms behind regenerative medicine and device-based therapies, evidence-informed candidacy criteria, and clear steps to book an evaluation. Current research through 2024 highlights growing support for selected regenerative and device therapies when combined with rehabilitation, and this guide translates that evidence into practical treatment choices. The sections below map causes to treatments, compare approaches including emerging alternatives, describe the specific services offered by Campbell Health Center, and finish with how to schedule the $49 consultation so you can move from information to action.
What Are the Common Causes of Knee Pain Treated Non-Surgically in Houston?
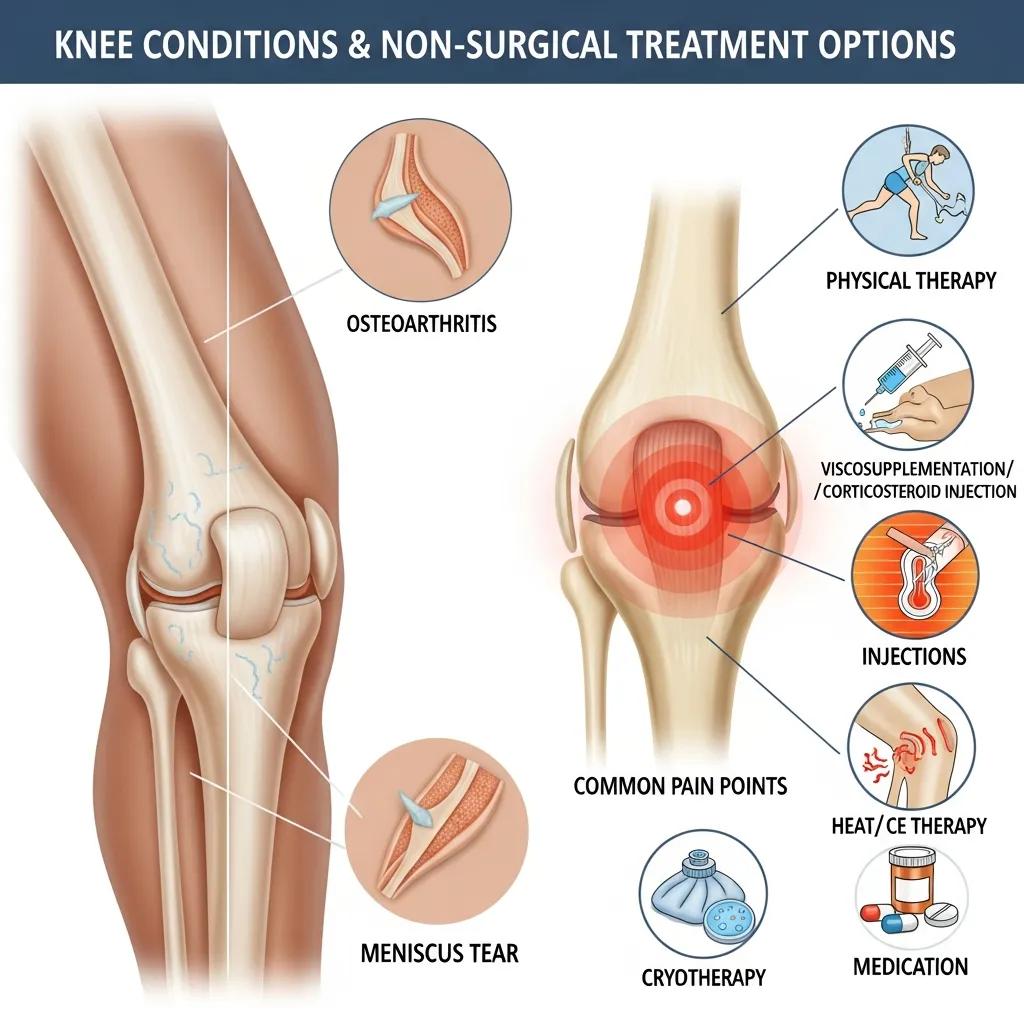
Non-surgical knee care targets a set of common conditions that produce pain through structural changes, inflammation, or biomechanical overload rather than catastrophic failure necessitating urgent surgery. Many chronic and subacute conditions—such as knee osteoarthritis, meniscus tears, tendinopathies, bursitis, and overuse syndromes—respond well to conservative and regenerative approaches that reduce inflammation and restore function. Understanding the underlying cause helps match treatment: cartilage-related pain favors regenerative injections and load management, while tendon pain often responds to shockwave or PRP plus targeted rehab. Knowing these distinctions empowers patients to choose appropriate non-surgical options and sets realistic expectations about recovery and timelines.
List of common non-surgically treated causes:
- Knee osteoarthritis: degenerative cartilage loss with joint inflammation and space narrowing.
- Meniscus tears: symptomatic tears that are small, stable, or degenerative can be managed conservatively.
- Tendonitis / tendinopathies: chronic tendon pain from overload that often responds to biologic or shockwave therapy.
- Bursitis and overuse syndromes: localized inflammation improved by activity modification and targeted therapies.
These causes overlap clinically, so an accurate history and focused exam guide the next step of imaging or targeted intervention, which we explore in the next subsection.
How Does Knee Osteoarthritis Cause Chronic Pain?
Knee osteoarthritis (OA) is a progressive condition in which articular cartilage thins, the synovial membrane becomes inflamed, and joint biomechanics change, producing pain during weight-bearing and reduced mobility. Mechanistically, cartilage loss exposes subchondral bone and alters load distribution, while low-grade inflammation from cytokines sustains pain and stiffness; together these create a cycle of degeneration and disability. Patients typically report activity-related pain that improves with rest early on but becomes more persistent as OA advances, affecting gait, stair negotiation, and recreational activity. Recent meta-analyses through 2024 emphasize that multimodal non-surgical care—exercise, load management, injections, and selective regenerative therapies—can reduce pain and improve function, especially when instituted early.
This pathophysiology frames why conservative strategies prioritize joint-preserving options and why regenerative approaches aim to modulate inflammation and support tissue repair in OA.
Regenerative and Pharmacologic Therapies for Osteoarthritis: Current Research and Future Directions
Osteoarthritis (OA) is a degenerative joint disorder commonly encountered in clinical practice, and is the leading cause of disability in elderly people. Due to the poor self-healing capacity of articular cartilage and lack of specific diagnostic biomarkers, OA is a challenging disease with limited treatment options. Traditional pharmacologic therapies such as acetaminophen, non-steroidal anti-inflammatory drugs, and opioids are effective in relieving pain but are incapable of reversing cartilage damage and are frequently associated with adverse events. Current research focuses on the development of new OA drugs (such as sprifermin/recombinant human fibroblast growth factor-18, tanezumab/monoclonal antibody against β-nerve growth factor), which aims for more effectiveness and less incidence of adverse effects than the traditional ones. Furthermore, regenerative therapies (such as autologous chondrocyte implantation (ACI), new generation of matrix-induced ACI, cell-free scaffolds, induced pluripotent stem cells (iPS cells or iPSCs), and endogenous cell homing) are also emerging as promising alternatives as they have potential to enhance cartilage repair, and ultimately restore healthy tissue. However, despite currently available therapies and research advances, there remain unmet medical needs in the treatment of OA. This review highlights current research progress on pharmacologic and regenerative therapies for OA including key advances and potential limitations.
Current research on pharmacologic and regenerative therapies for osteoarthritis, W Zhang, 2016
What Other Knee Conditions Can Benefit from Non-Surgical Treatments?
Beyond OA, several injury and overuse conditions commonly respond to non-operative care, including small degenerative meniscus tears, partial ligament sprains, chronic patellar tendinopathy, and iliotibial-band related runner’s knee. These conditions often share a mechanical or inflammatory driver—overload, malalignment, or repetitive strain—that responds well to rehabilitation, bracing, targeted injections like PRP, and device therapies such as shockwave or PEMF. Clinicians typically reserve surgery for large structural failures, entrapped meniscal flaps, or instability after failed conservative care, while many patients achieve meaningful symptom relief without an operation. Early appropriate intervention can shorten recovery and reduce the likelihood of disease progression.
Knowing which diagnosis aligns with which non-surgical pathway helps patients pursue effective, less invasive management before considering surgical options.
Degenerative Meniscus Tears: Understanding Pathogenesis, Diagnosis, and Non-Surgical Treatment Options
The symptomatic degenerative meniscus continues to be a source of discomfort for a significant number of patients. With vascular penetration of less than one-third of the adult meniscus, healing potential in the setting of chronic degeneration remains low. Continued hoop and shear stresses upon the degenerative meniscus results in gross failure, often in the form of complex tears in the posterior horn and midbody. Patient history and physical examination are critical to determine the true source of pain, particularly with the significant incidence of simultaneous articular pathology. Joint line tenderness, a positive McMurray test, and mechanical catching or locking can be highly suggestive of a meniscal source of knee pain and dysfunction. Radiographs and magnetic resonance imaging are frequently utilized to examine for osteoarthritis and to verify the presence of meniscal tears, in addition to ruling out other sources of pain. Non-operative therapy focused on non-steroidal an
Degenerative meniscus: Pathogenesis, diagnosis, and treatment options, 2014
Why Choose Non-Surgical Knee Pain Relief Options in Houston?
Non-surgical knee care emphasizes preserving the native joint, reducing risk, and promoting natural healing processes that often lead to shorter recovery and fewer complications than surgery. These approaches minimize exposure to anesthesia and hospitalization, lower infection and complication risk, and aim to restore function through biological modulation or mechanical rebalancing. Recent guidelines recommend attempting conservative and targeted regenerative strategies before elective joint replacement in many patients, particularly those seeking to maintain active lifestyles. For patients concerned about durability and safety, non-surgical options can be sequenced—starting with rehabilitation and progressing to injections or device-based therapies—so care is individualized and data-driven.
For patients who want a clinic focused on root-cause care and avoiding unnecessary procedures, Campbell Health Center emphasizes safe, natural treatments and a patient-first pathway; learn more about the clinic’s service menu in the treatment section below, and consider the $49 consultation to review your options.
What Are the Benefits of Avoiding Knee Surgery?
Avoiding or delaying knee surgery offers several clear patient-centered advantages, including reduced recovery time, fewer perioperative risks, and preservation of native joint anatomy which can simplify future interventions if needed. Non-surgical care usually allows faster return to daily activities and work, and it avoids risks like surgical-site infection, anesthesia complications, and prolonged rehabilitation associated with joint replacement. Additionally, many non-operative interventions can be repeated, combined, or adjusted over time to respond to symptom changes without irreversible alteration to the joint. These benefits make conservative-first strategies attractive for patients who prioritize function, lower immediate risk, and preserving future surgical options.
Understanding these benefits helps patients weigh trade-offs between immediate surgical correction and staged conservative care that aims to restore function with lower risk.
How Do Non-Surgical Treatments Promote Natural Healing?
Non-surgical treatments promote natural healing through diverse biological and mechanical mechanisms: PRP delivers concentrated growth factors that modulate inflammation and stimulate repair; stem cells and regenerative cellular tissue therapies aim to provide trophic support and a favorable microenvironment for tissue maintenance; shockwave therapy induces microtrauma and neovascularization to remodel chronic tendon pathology; PEMF alters cellular signaling to reduce pain and support repair; and chiropractic and rehabilitation address biomechanics to offload injured tissues. Each mechanism translates into symptom reduction, improved strength or tissue quality, and better function when paired with exercise and load management. Recent clinical evidence through 2024 supports these mechanisms for selected indications, though treatment choice depends on diagnosis and patient goals.
These mechanistic insights guide matched therapy selection and set expectations about timelines and likely outcomes for each modality.
What Advanced Non-Surgical Treatments for Knee Pain Does Campbell Health Center Offer?
Campbell Health Center offers a menu of advanced non-surgical options organized under regenerative medicine and pain-relief services designed to reduce pain and support healing without surgery. Regenerative injections (PRP, stem cell and regenerative cellular tissue therapies) aim to modulate inflammation and promote tissue repair; device-based treatments (shockwave, PEMF) stimulate localized healing responses; chiropractic care and spinal decompression restore biomechanics and address nerve-related contributors; and all services are integrated into individualized plans that prioritize avoiding unnecessary surgery. Below we define the major options, describe mechanisms and candidate profiles, and provide a compact comparison to help patients choose suitable approaches.
The following EAV table compares core treatments offered, their mechanisms, and ideal candidates to clarify options and guide decision-making.
| Treatment | Mechanism | Clinical Benefit / Ideal Candidate |
|---|---|---|
| Platelet-Rich Plasma (PRP) | Autologous platelet concentration releases growth factors | Reduces tendon inflammation and aids soft-tissue healing; ideal for chronic tendinopathy and select meniscal pathology |
| Stem Cell / Regenerative Cellular Tissue | Cellular and trophic factors modulate inflammation and tissue environment | Aims to support cartilage preservation and symptomatic OA relief in selected patients seeking regenerative options |
| Shockwave Therapy | Focused acoustic waves stimulate neovascularization and tissue remodeling | Effective for chronic tendinopathies and select enthesopathies; good for patients unresponsive to rehab |
| PEMF Therapy | Electromagnetic fields alter cellular signaling and pain pathways | Adjunct for pain modulation and accelerated recovery in post-procedure or chronic pain states |
| Chiropractic Care | Manual adjustment and biomechanical correction | Helps restore joint mechanics and offload symptomatic areas; suitable as adjunct to regenerative care |
| Spinal Decompression | Mechanical traction to relieve nerve root compression | Used when nerve-related knee symptoms originate in lumbar pathology; appropriate for radicular knee pain patterns |
This comparison helps patients and clinicians align symptoms and goals with specific therapies; the next subsections explain regenerative principles and how combination care is applied.
How Does Regenerative Medicine Work for Knee Pain Relief?

Regenerative medicine uses biologic agents to alter the joint environment, reduce harmful inflammation, and support intrinsic repair processes rather than masking symptoms alone. Mechanistically, injected biologics deliver growth factors, cytokine modulators, and cellular components that shift the balance from catabolic to reparative signaling within the joint or around tendons. Clinically, this can produce gradual pain reduction, improved mobility, and reduced reliance on analgesics over weeks to months, and outcomes are typically optimized when combined with targeted rehabilitation and load modification. Current research through 2024 supports selected regenerative approaches for symptomatic relief in osteoarthritis and chronic tendinopathies in carefully selected patients.
Explaining regenerative mechanisms clarifies why treatment plans often sequence injections with rehab and adjunctive device therapies for best results.
Minimally Invasive Cellular Therapies for Osteoarthritis: A Novel Approach to Cartilage Regeneration
Osteoarthritis (OA) is a chronic degenerative disease characterized by multiple pathological conditions such as synovitis, degeneration of the articular cartilage, subchondral bone remodeling, and osteophyte formation. Local chronic inflammation response induces degradation of cartilage and the poor regenerative ability of articular cartilage due to its avascular nature and limited regeneration of chondrocytes affecting the microenvironment of the joint. Current clinical treatments provide temporal pain relief but have failed to treat OA pathogenesis. In addition, surgical invasive methods have the risk of adverse complications such as long-term pain and increased morbidity. Therefore, there is a need to develop novel therapeutic strategies to prevent adverse effects seen in current surgical approaches. Minimally invasive therapies have been explored to overcome the limitations of conventional OA therapies. In recent years, cellular-based therapies have been employed to suppress inflammation and promote cartilage regeneration by using progenitor cells and stem cells including induced pluripotent stem cells (iPSCs) and genetically modified cells. The present review summarizes the status of cellular-based therapy for OA treatment. We suggest that minimally invasive intervention in the microenvironment of the joint may overcome the current limitation for OA treatment.
Minimally invasive cellular therapies for osteoarthritis treatment, S Shah, 2021
What Are the Roles of PRP, Stem Cell, and Regenerative Cellular Tissue Therapies?
PRP, stem cell, and regenerative cellular tissue therapies differ by source material and intended biological effect: PRP uses a patient’s platelets to concentrate growth factors that reduce inflammation and support tendon and soft-tissue healing; stem cell and regenerative cellular tissue therapies aim to provide a broader set of trophic factors to influence cartilage and complex tissue environments. PRP is commonly indicated for tendinopathies, milder meniscal symptoms, and select early osteoarthritis, while regenerative cellular therapies are considered for patients seeking stronger trophic modulation for cartilage-related symptoms. Safety profiles are generally favorable when performed under clinical protocols, but evidence strength varies by indication, and patients should be counseled about realistic symptom timelines and the need for adjunctive rehabilitation.
A clear understanding of these differences helps patients choose the right biologic for their diagnosis and goals.
How Do Chiropractic Care, Shockwave, PEMF, and Spinal Decompression Therapies Help Knee Pain?
Non-injection modalities play important adjunctive roles: chiropractic care improves joint alignment and lower-extremity biomechanics to reduce abnormal load on the knee; shockwave therapy stimulates localized tissue repair and is effective for chronic tendinopathies; PEMF provides noninvasive cellular modulation that can ease pain and support recovery after procedures; and spinal decompression addresses lumbar-origin radicular patterns that can present as knee pain. Each therapy can be used alone for specific problems or combined into a multimodal plan to address both symptoms and contributing biomechanical factors. Selection depends on diagnosis, prior treatments, and patient preference, with many patients benefiting from combined biomechanical correction plus biologic therapy.
These device and manual options broaden non-surgical pathways and improve the likelihood of durable symptom control when appropriately matched.
How Are Specific Knee Conditions Treated Without Surgery in Houston?
Mapping diagnoses to evidence-based non-surgical interventions helps patients understand typical outcomes and timelines, and clarifies when imaging or referral is warranted. For knee osteoarthritis, first-line care emphasizes exercise, weight management, bracing, and targeted injections, with regenerative options considered when conservative measures fail to deliver adequate relief. Meniscal tears and partial ligament sprains often follow rehabilitation protocols and selective injections if healing is delayed, while runner’s knee and bursitis typically respond to activity modification, shockwave, and PRP when chronic. It is important to recognize red flags—severe instability, locked knee, or systemic signs—that require urgent evaluation and possible surgical referral.
The EAV table below maps common knee conditions to non-surgical options and expected recovery timelines to set realistic expectations.
| Knee Condition | Non-Surgical Options | Typical Outcomes / Timeline |
|---|---|---|
| Osteoarthritis | Exercise therapy, bracing, weight loss, corticosteroid/PRP/regenerative injections | Symptom reduction weeks–months; functional gains with sustained rehab |
| Meniscus Tear (degenerative/small) | Physical therapy, activity modification, PRP for symptomatic relief | Many improve in 6–12 weeks; imaging guides escalation |
| Partial Ligament Sprain | Rehab, bracing, gradual strengthening, possible biologic adjuncts | Return to activity in 8–12 weeks with structured rehab |
| Runner’s Knee / Bursitis | Load modification, targeted PT, shockwave, PRP if chronic | Symptom relief 4–12 weeks depending on chronicity |
What Non-Surgical Options Are Available for Knee Osteoarthritis?
Knee OA management in non-surgical practice starts with exercise therapy, weight management, bracing as indicated, and activity modification to reduce symptomatic load on the joint. Pharmacologic and injection options—such as corticosteroids for short-term flare control and PRP or regenerative options for longer-term symptom modulation—are used selectively based on goals and evidence. Rehabilitation and structured exercise programs are foundational and often combined with regenerative injections to optimize outcomes, with expected symptomatic improvements over weeks to months. Recent clinical guidance through 2024 recommends shared decision-making and sequencing conservative measures before considering joint replacement for many patients.
This staged approach balances immediate symptom control with longer-term joint preservation strategies.
How Are Meniscus Tears and Ligament Injuries Managed Non-Surgically?
Small, degenerative meniscal tears and partial ligament sprains frequently improve with a structured rehabilitation program focused on strengthening, range-of-motion, and neuromuscular control, while injections like PRP can be considered for persistent symptomatic cases. Decision-making weighs tear size, mechanical symptoms (locking or catching), instability, and patient activity goals; when mechanical derangement is absent, conservative care is often successful. Recovery benchmarks typically range from 6 to 12 weeks for symptomatic improvement, with gradual return to activity guided by functional milestones rather than fixed timelines. Imaging and specialist referral remain important when symptoms persist or when mechanical problems emerge.
This conservative-first strategy preserves options and emphasizes functional recovery when surgery is not immediately required.
What Are the Treatments for Runner’s Knee and Bursitis Without Surgery?
Runner’s knee and bursitis respond well to activity modification, progressive strengthening of hip and knee stabilizers, soft-tissue therapies, and targeted device or biologic treatments for chronic cases. Initial care includes relative rest, anti-inflammatory strategies, and a supervised exercise program to correct biomechanical contributors; chronic or refractory cases may benefit from shockwave therapy or PRP to jump-start tissue remodeling. Patient education on training load, footwear, and cross-training are essential components of durable recovery. These practical measures often restore pain-free function and prevent recurrence when consistently applied.
Addressing biomechanical and training factors is central to preventing relapse and optimizing long-term outcomes.
Who Is an Ideal Candidate for Non-Surgical Knee Pain Treatment in Houston?
Ideal candidates for non-surgical knee care are patients with pain driven by degenerative change, tendinopathy, or minor structural lesions without severe deformity or advanced, irreversible joint destruction that mandates joint replacement. Good candidates typically have realistic functional goals, willingness to engage with rehabilitation, and the absence of red-flag symptoms such as uncontrolled infection, progressive neurological deficit, or an acutely locked joint. Comorbidities and prior surgeries influence choice and sequencing of therapies, and treatment plans are adjusted to balance safety and expected benefit. Clear expectation-setting helps patients understand likely timelines and the possibility that surgery may be required if conservative care fails.
To clarify candidacy factors and how they change treatment choice, see the EAV table below.
| Patient Factor | Why It Matters | Treatment Implication |
|---|---|---|
| Symptom Pattern (activity-related vs constant) | Suggests mechanical vs inflammatory driver | Activity-related pain favors rehab and load management; constant severe pain may need imaging |
| Imaging Findings (mild vs severe OA) | Degree of structural change predicts response | Mild–moderate OA often responds to regenerative + rehab; advanced OA may require joint replacement |
| Prior Treatments | Prior failures guide escalation | Failed rehab/meds may prompt biologic or device-based interventions |
| Comorbidities | Safety and healing capacity affected | Certain conditions may limit procedural options or alter timelines |
What Should Patients Expect During Their Consultation?
During the $49 consultation patients receive a focused history, a targeted physical exam, and review of any prior imaging to create an individualized treatment plan that prioritizes conservative, joint-preserving options. The clinician discusses diagnosis, realistic goals, recommended next steps—such as supervised rehabilitation, injections, or device therapies—and provides an estimated timeline and cost framework for proposed interventions. Patients leave with a clear plan that sequences therapies logically, explains risks and benefits, and identifies measurable functional milestones for follow-up. This structured assessment supports informed decision-making and avoids unnecessary procedures by emphasizing conservative-first pathways.
The consult’s clarity and shared planning make it easier for patients to commit to a stepwise treatment approach.
How Does Campbell Health Center Personalize Treatment Plans?
Campbell Health Center personalizes plans by integrating diagnostic findings, patient goals, activity level, and previous care into a multimodal strategy that may combine regenerative injections, device therapies, manual care, and rehab. Practitioners tailor modalities—choosing PRP for tendon-driven pain, regenerative cellular tissue for select OA presentations, or shockwave for chronic tendinopathy—and schedule follow-ups to monitor progress and adapt the plan. Personalization also considers practical factors like insurance independence and patient preference for natural, root-cause focused care. This individualized approach aims to maximize non-surgical benefit while keeping the door open for other options if conservative measures do not meet goals.
Personalized sequencing and active monitoring increase the likelihood of meaningful, durable improvements without immediate surgery.
How Can You Schedule a Consultation for Non-Surgical Knee Pain Relief at Campbell Health Center?
Scheduling begins with a clear set of steps so patients can move efficiently from concern to evaluation and an evidence-based plan. The center offers a $49 consultation that covers history, focused exam, and review of available imaging, followed by a discussion of recommended non-surgical options and next steps. Campbell Health Center operates independently of insurance and Medicare, which allows flexibility in treatment selection and pricing transparency for regenerative and pain-relief services. To prepare for the visit, gather prior imaging, a concise symptom history, and a list of medications so the team can create the most effective, individualized plan during the consultation.
Below is a simple step-by-step guide for booking and preparing that mirrors what patients will experience.
- Gather Records: Bring recent imaging and current medication list to the consult.
- Call to Schedule: Use the clinic contact to request the $49 consultation and state your primary knee concern.
- Prepare Goals: Write down activity and functional goals to discuss during the appointment.
- Attend Focused Visit: Expect history, exam, imaging review, and a clear recommended plan within the consultation.
What Does the $49 Consultation Include?
The $49 consultation includes a thorough patient history, a focused musculoskeletal exam, and review of any prior imaging to accurately diagnose the probable pain generators and outline evidence-informed non-surgical options. During the visit clinicians explain likely timelines, risks, and expected functional outcomes for each recommended therapy and provide a written plan that sequences rehabilitation, injections, or device services as appropriate. The fee covers evaluation and planning; any procedural or therapy costs are discussed separately when a treatment decision is made. This transparent approach helps patients understand both clinical and financial implications before committing to interventions.
Clear pre-visit communication about what the consultation covers reduces uncertainty and supports informed consent for subsequent treatments.
How to Prepare for Your First Visit to Campbell Health Center?
Preparing for your first visit maximizes value: bring prior imaging studies (X-rays, MRI), a current medication list, and a concise symptom timeline describing onset, aggravating/alleviating factors, and functional limitations. Wear comfortable clothing to allow a focused knee exam and be ready to discuss prior treatments and goals for mobility or sport participation. Preparing questions about non-surgical alternatives, timelines, and expected outcomes helps ensure the consultation addresses your priorities. Arriving organized allows the clinician to rapidly tailor a personalized plan and recommend next steps that aim to improve function without unnecessary surgery.
A prepared patient leaves the consult with clear guidance and a realistic plan that fits their goals and circumstances.
| Preparation Item | Purpose | Tip |
|---|---|---|
| Prior imaging | Confirms structural diagnosis | Bring digital or printed images/reports |
| Medication list | Safety and interaction review | Include supplements and OTC meds |
| Symptom diary | Clarifies pain patterns | Note activities that worsen or improve pain |
| Functional goals | Guides personalized plan | State desired activities (e.g., walking, running) |
For patients in Houston seeking safe, natural, and individualized non-surgical knee care, the steps above map a practical route from diagnosis to multimodal, evidence-informed treatment pathways designed to reduce pain and preserve function. Campbell Health Center’s clinic-based services emphasize regenerative medicine and multimodal pain relief, and the $49 consultation provides a low-cost entry point to review options and begin a conservative-first plan tailored to each patient’s needs.








