
Non-Surgical Knee Pain Treatment in Houston: How Innovative Therapies Are Changing Lives
Knee pain in Houston affects people across ages and activity levels, and non-surgical knee pain treatments offer effective, less invasive ways to reduce pain, restore function, and delay or avoid joint replacement. This article explains common causes and symptom patterns for knee pain, summarizes the mechanisms behind leading non-surgical options such as platelet rich plasma (PRP), stem cell therapy, genicular artery embolization (GAE), and viscosupplementation, and provides practical guidance on choosing treatments. Readers will learn how regenerative medicine and energy-based therapies work, who is most likely to benefit, and what recovery looks like for each approach. The piece also compares non-surgical pathways to surgical alternatives, presents an easy-to-follow decision framework, and outlines how a Houston clinic personalizes care. Finally, you’ll find patient-focused success stories and concise answers to frequently asked questions that help guide the next step toward relief from knee pain in Houston.
What Are the Common Causes and Symptoms of Knee Pain in Houston?
Knee pain in Houston commonly arises from structural degeneration, acute injury, biomechanical overload, or referred pain from the spine; each cause produces a distinct symptom pattern that helps clinicians target treatment. Mechanical wear like osteoarthritis creates ache and stiffness with activity, while meniscal or ligament injuries cause sharp pain, swelling, and instability. Chronic overuse and alignment problems produce gradual-onset pain and intermittent swelling, and neuropathic contributors can create burning or electric sensations. Understanding the pattern of pain, timing, and functional limitations is the first step toward choosing a non-surgical strategy that addresses the underlying problem and not only symptoms.
Knee pain can also vary by activity and context, so clinicians evaluate onset, aggravating movements, and prior treatments to map the problem accurately. This evaluation guides imaging choices and treatment sequencing, and it helps patients set realistic goals for mobility and pain reduction. Recognizing red flags—fever, rapidly worsening swelling, or inability to bear weight—ensures timely referral when urgent care or surgical evaluation is required. With those diagnostic distinctions in mind, we next examine how osteoarthritis and joint wear specifically drive chronic knee pain.
How Does Osteoarthritis and Joint Wear Affect Knee Pain?
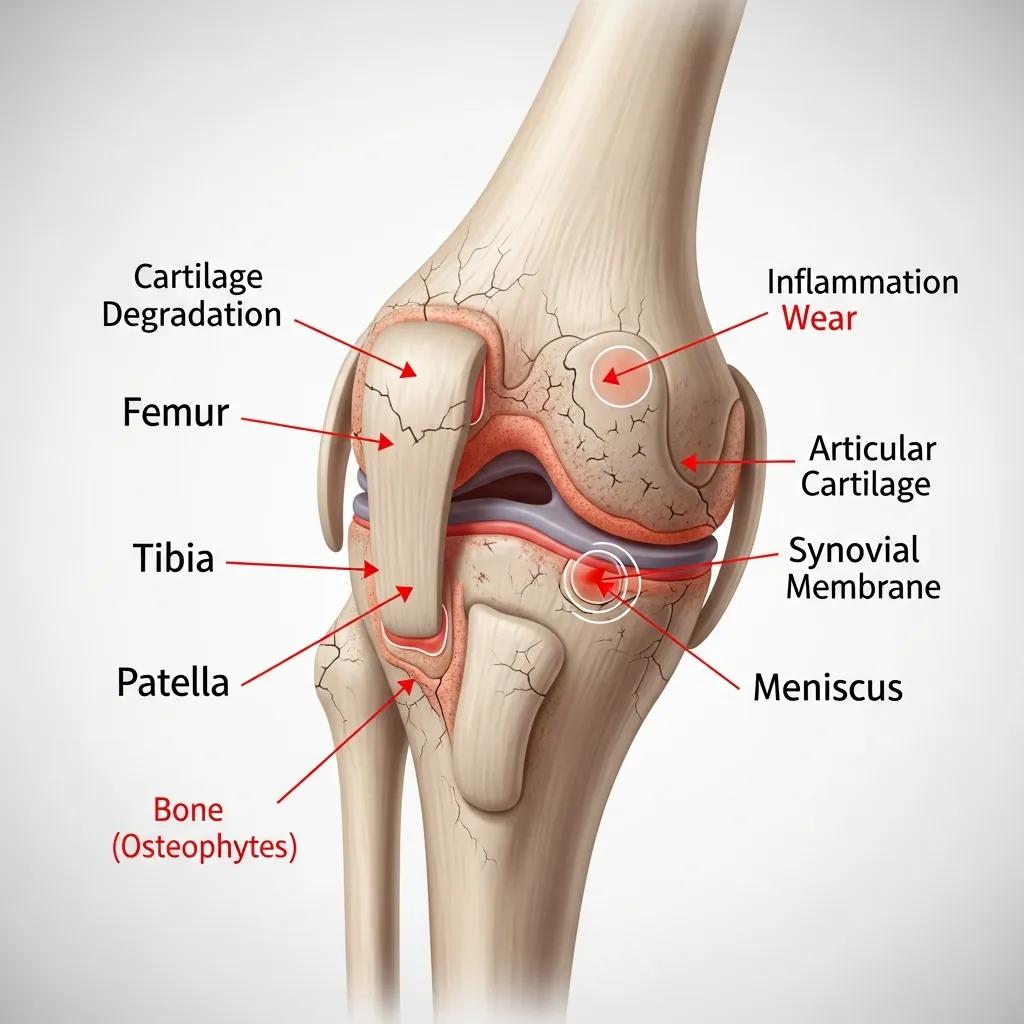
Osteoarthritis (OA) is joint cartilage breakdown that produces pain through increased bone-on-bone contact, inflammation, and altered joint mechanics; this process explains why activity, weight-bearing, and humidity changes can trigger symptoms. Cartilage loss reduces shock absorption, which increases stress on subchondral bone and synovium, provoking inflammatory mediators that amplify pain and stiffness. Patients typically report morning stiffness that improves with gentle movement and pain with prolonged standing or stairs; these clinical features influence which non-surgical therapies are most appropriate. Treatments like viscosupplementation, PRP, and genicular artery embolization target inflammation, lubrication, and abnormal pain signaling respectively, offering symptom relief without replacing the joint.
Clinicians assess OA stage, alignment, and cartilage status through exam and imaging to match treatments to pathology and patient goals. Early-stage OA may respond well to regenerative approaches that modulate inflammation and encourage tissue repair, while advanced degeneration might require combination strategies to manage pain and function. Understanding OA mechanics leads directly into a discussion of how chronic knee pain impacts everyday life and why timely non-surgical intervention matters.
What Impact Does Chronic Knee Pain Have on Daily Life?
Chronic knee pain reduces mobility, limits work and household tasks, and often causes secondary effects such as sleep disruption, mood changes, and decreased cardiovascular fitness due to activity avoidance. Patients commonly report difficulty with stairs, walking longer distances, and participating in recreational activities, which can lead to weight gain that further stresses the joint. These functional and psychosocial impacts increase the urgency of early, effective treatment that preserves joint structure and restores activity. Addressing pain proactively with non-surgical options can interrupt the cycle of deconditioning and progressive disability, improving quality of life and reducing long-term healthcare burden.
Behavioral and rehabilitative elements—strength training, gait correction, and graded activity—are vital complements to procedural therapies, because restoring biomechanics reduces re-injury risk and sustains gains. This emphasis on combined care leads to the next section where we compare non-surgical approaches against surgical alternatives.
Why Choose Non-Surgical Treatments for Knee Pain in Houston?
Non-surgical knee pain treatments offer targeted symptom relief, lower complication risks, and shorter recovery windows compared with joint replacement, while preserving the native joint for future options. Regenerative therapies like PRP and stem cell interventions aim to modulate inflammation and support tissue repair, whereas procedures such as genicular artery embolization reduce pain signaling without altering joint anatomy. Energy-based and biomechanical treatments, including shockwave therapy, PEMF, chiropractic care, and Knee on Trac, address tendinopathy, cellular healing, and alignment. For many patients the cumulative benefit is meaningful pain reduction with faster return to activity and fewer disruptions to daily life.
When evaluating surgical versus non-surgical paths, patients and clinicians weigh risks, expected recovery time, and long-term outcomes to select the best course for the individual’s goals and anatomy. Non-surgical options are particularly attractive for patients who want to avoid prosthesis-related limitations or who are not ideal surgical candidates. Next we summarize the main comparative dimensions that help patients decide between these pathways.
Different approaches emphasize distinct advantages:
- Lower risk profile: Minimally invasive procedures typically have fewer systemic complications than major surgery.
- Shorter downtime: Many non-surgical procedures allow earlier return to work and daily activities.
- Joint preservation: Treatments focus on maintaining native tissue and function where possible.
These comparative benefits lead into a structured table contrasting surgery and non-surgical options for clear decision-making.
Non-surgical and surgical approaches differ in predictable ways that guide treatment planning.
| Approach | Typical Risks | Typical Recovery | Long-term Considerations |
|---|---|---|---|
| Joint replacement (surgical) | Anesthesia risks, infection, prosthesis wear | Weeks to months, physical therapy required | Durable pain relief for many, but prosthesis lifespan limits repeat options |
| Regenerative therapies (PRP, stem cells) | Local reaction, transient pain increase | Days to weeks, progressive improvement over months | Aimed at symptom reduction and tissue modulation; repeat treatments possible |
| Endovascular (GAE) | Vascular procedure risks, local discomfort | Short outpatient recovery, rapid pain decrease in many cases | Can reduce pain without altering joint mechanics |
| Injections (steroid, hyaluronic acid) | Local infection, steroid effects | Short-term relief days–months | Useful as part of multimodal plan, often temporary relief |
This comparison clarifies why many patients pursue non-surgical paths first, and it sets up the detailed descriptions of available therapies in the next section.
Which Non-Surgical Knee Pain Treatments Are Available in Houston?
A broad spectrum of non-surgical options is available in Houston, ranging from biologic injections to mechanical therapies and endovascular procedures; each addresses different pain mechanisms and patient needs. Platelet rich plasma (PRP) and stem cell therapies act through biologic modulation and tissue-supporting signals, joint injections and viscosupplementation focus on lubrication and inflammation control, while genicular artery embolization (GAE) targets abnormal pain-carrying blood vessels. Shockwave and PEMF therapies stimulate tissue repair via mechanical or electromagnetic signals, and chiropractic, spinal decompression, Knee on Trac, and rehabilitation address alignment, mechanical load distribution, and functional restoration. Understanding these categories helps match the therapy to the underlying problem and patient goals.
| Treatment | Mechanism | Typical Benefits | Downtime |
|---|---|---|---|
| PRP (Platelet Rich Plasma) | Growth factor delivery from patient’s blood | Reduced inflammation, improved function over months | Minimal; a few days of soreness |
| Stem Cell Therapy | Cellular and paracrine signaling to support repair | Potential tissue support and pain reduction | Minimal to moderate; short recovery period |
| Joint Injections (steroid, hyaluronic acid) | Anti-inflammatory or lubricating effect | Rapid pain relief (steroids) or improved glide (HA) | Hours to days; steroids limited frequency |
| Genicular Artery Embolization (GAE) | Reduces abnormal arterial flow sustaining pain | Durable pain reduction for select OA patients | Short outpatient recovery, days of soreness |
| Shockwave Therapy | Mechanical stimulation of soft-tissue healing | Tendon and soft-tissue pain improvement over weeks | Minimal downtime; repeated sessions |
| PEMF Therapy | Electromagnetic stimulation of cellular processes | Support for healing and pain modulation | No downtime; multiple sessions |
This table illustrates how each option fits different clinical needs. Campbell Health Center provides many of these services as part of its non-surgical menu in Houston and evaluates patients to determine which therapies are appropriate based on symptoms, imaging, and functional goals. After explaining specific therapies below, we describe how a personalized plan is formulated.
How Does Platelet Rich Plasma Therapy Relieve Knee Pain?
Platelet rich plasma (PRP) therapy uses a concentrated sample of the patient’s own platelets, which release growth factors that modulate inflammation and support tissue repair, making PRP a biologic option for osteoarthritis and soft-tissue injuries. The procedure involves a blood draw, centrifugation to isolate platelets, and image-guided injection into the affected knee; most patients experience transient soreness followed by gradual improvement over weeks to months. PRP typically requires one to three sessions spaced weeks apart depending on the condition and provider protocol, and its evidence base shows benefit for many patients compared with placebo for certain OA grades. Side effects are usually mild and limited to local pain or swelling, and recovery focuses on activity modification and progressive rehabilitation.
The effectiveness of intra-articular PRP injections in the knee joint is supported by research, which discusses its molecular mechanisms of action and degree of efficacy.
Platelet-Rich Plasma Injections for Knee Osteoarthritis: Mechanisms and Efficacy
Platelet-rich plasma (PRP) has lately been investigated for the treatment of knee OA. This article reviews recent molecular mechanisms of action. The effectiveness of intra-articular PRP injections in the knee joint is discussed.
Understanding PRP’s mechanism clarifies why it is often combined with physical therapy to restore biomechanics and maximize functional gains after biologic modulation.
What Role Does Stem Cell Therapy Play in Knee Pain Management?
Stem cell therapy aims to provide cellular signaling that supports tissue repair and reduces inflammation in degenerative knee conditions, using cells or regenerative cellular tissue to influence the joint environment. The clinic process typically includes patient evaluation, sourcing of regenerative cellular tissue per protocol, and targeted injection into damaged areas; patients generally follow a rehabilitation plan to support tissue integration and function. Outcomes vary by patient and by the specific regenerative product used, with many reporting gradual functional improvement over several months rather than immediate relief. Risks are generally local and procedure-related; candidacy is determined through clinical assessment and imaging to set realistic expectations.
Research has systematically reviewed randomized controlled trials to assess the efficacy and safety of autologous stem cell therapy compared to other treatments or placebo in patients with knee osteoarthritis.
Autologous Stem Cell Therapy for Knee Osteoarthritis: Efficacy and Safety Review
Autologous stem cell therapy compared with any other treatment or placebo in patients with KOA on patient-reported outcome measures. The review aims to assess the efficacy and safety of autologous stem cell therapy compared with any other treatment or placebo in patients with KOA on patient-reported outcome measures.
Given variability in response, clinicians emphasize careful selection and combined rehabilitation to enhance the chance of meaningful improvement.
How Do Joint Injections Help with Knee Arthritis Relief?
Joint injections include corticosteroids for rapid anti-inflammatory effect and hyaluronic acid (viscosupplementation) to improve joint lubrication; both are useful tools in managing arthritis-related pain as part of a broader plan. Steroid injections can provide quick pain relief lasting weeks to months but are limited in frequency due to potential cartilage effects, whereas viscosupplementation aims to improve joint glide and may provide more gradual symptom relief. Nerve-targeted injections and local anesthetic blocks can be diagnostic and temporarily therapeutic, guiding further care. Integrating injections with regenerative therapies and rehabilitation often yields better functional outcomes than injections alone.
Clinicians balance immediate symptom control with long-term joint preservation when recommending injection timing and type, and they may sequence injections alongside PRP or stem cell treatments for optimized effect.
What Are the Benefits of Chiropractic Care and Shockwave Therapy for Knee Pain?
Chiropractic care focuses on alignment, biomechanical correction, and soft-tissue work to reduce abnormal load on the knee, while shockwave therapy applies focused mechanical energy to stimulate tendon and soft-tissue healing. Chiropractic interventions can improve gait, redistribute forces across the joint, and reduce compensatory strain in surrounding tissues, supporting long-term function. Shockwave is often used for tendinopathies and insertional pain and can reduce pain and improve tendon structure over a series of sessions. Combining manual care with regenerative or injection therapies enhances outcomes by addressing both biological and mechanical contributors to pain.
These conservative modalities are frequently integrated into multi-modal plans that emphasize tissue healing plus biomechanical correction for durable improvement.
How Do Advanced Treatments Like PEMF Therapy and Spinal Decompression Work?
PEMF (pulsed electromagnetic field) therapy delivers low-intensity electromagnetic pulses intended to influence cellular signaling and promote healing processes, while spinal decompression relieves disc-related or nerve-compression issues that can refer pain to the knee. PEMF aims to modulate inflammation and cellular repair, often used as an adjunct across multiple sessions with minimal risk and no downtime. Spinal decompression addresses biomechanical contributors and is considered when lumbosacral pathology contributes to knee pain through referred pathways or altered gait mechanics. Both approaches fit into comprehensive care models that pair local knee treatments with broader neuromuscular rehabilitation to maximize functional recovery.
Combining local biologic treatments with systemic or spinal interventions helps ensure that both primary knee pathology and secondary contributors are managed effectively.
What Is Genicular Artery Embolization and How Does It Help Knee Pain?
Genicular artery embolization (GAE) is a minimally invasive outpatient procedure that selectively reduces abnormal arterial flow to pain-generating regions of an osteoarthritic knee, thereby decreasing persistent inflammatory signaling and pain. The intervention uses image-guided catheter techniques to deliver embolic material to targeted genicular branches, and many patients experience meaningful pain reduction within weeks with a short recovery period. Ideal candidates are those with symptomatic knee OA who prefer to avoid joint replacement and who have pain patterns consistent with vascular-mediated inflammatory contributors. Limitations include patient-specific vascular anatomy and the need for careful selection by interventional specialists.
Studies suggest that Genicular Artery Embolization (GAE) shows promising results for treating osteoarthritis-related knee pain, with most treatments demonstrating durable clinical responses.
Genicular Artery Embolization for Knee Pain: Promising Results for Osteoarthritis
ConclusionLimited single-arm studies report GAE is promising for treating OA-related pain. Most treatments performed for mild-to-moderate OA demonstrated durable clinical responses from 6 months to 4 years. Limited data for severe OA suggest a non-durable response. Future studies should be standardized to facilitate comparison and control for placebo effect.
GAE expands the toolkit for managing OA-related pain when other conservative measures have been insufficient, and it frequently pairs with rehabilitation to maintain mobility gains.
How Does Campbell Health Center Personalize Non-Surgical Knee Pain Care in Houston?
Campbell Health Center personalizes knee pain care through a structured three-step approach: a focused consultation and evaluation, a custom healing plan that blends regenerative and conservative modalities, and ongoing tracking to help patients regain function. The clinic operates independently of insurance and Medicare, which allows clinicians to prioritize the most appropriate evidence-based options for each patient without coverage-driven constraints. For initial access, Campbell Health Center offers a $49 consultation that includes a clinical evaluation and X-rays to inform candidacy for therapies and create a tailored plan. This patient-centered model emphasizes transparency, individualized therapy sequencing, and measurable outcome tracking to support long-term improvement.
- Consultation & Evaluation: Comprehensive exam and X-rays included with the $49 consult to clarify diagnosis and goals.
- Custom Healing Plan: A tailored mix of regenerative, injection-based, mechanical, and rehabilitative therapies selected to address the patient’s specific pathology.
- Regain Your Freedom: Ongoing monitoring, functional milestones, and adjustments to therapy to sustain gains and return to desired activities.
This independent, transparent pathway reduces scheduling delays and enables clinicians to recommend the best combination of services—such as PRP, stem cell options, joint injections, GAE, shockwave, PEMF, chiropractic care, spinal decompression, viscosupplementation, and Knee on Trac therapy—based on the patient’s needs. To explore candidacy or book the $49 consultation, patients can contact Campbell Health Center by phone or visit the clinic at the provided address to begin their personalized plan.
What Are Patient Success Stories After Non-Surgical Knee Pain Treatments in Houston?

Patients in Houston who pursue non-surgical knee pain treatments often report measurable improvements in pain scores and functional milestones such as climbing stairs, walking longer distances, and returning to recreational activities within months. Case vignettes highlight individuals who avoided surgery by combining PRP or stem cell therapy with a rehabilitative program, showing progressive pain reduction and increased walking tolerance over 8–12 weeks. Other patients treated with GAE report rapid reductions in activity-limiting pain with quick return to daily tasks, while those receiving viscosupplementation or shockwave therapy note improved joint mobility that supports ongoing strengthening. These structured outcomes demonstrate that individualized, multi-modal non-surgical plans can restore meaningful function without joint replacement.
Patient experiences emphasize the role of rehabilitation and realistic timelines, underscoring that procedural therapies typically require follow-up therapy and graded activity to achieve lasting benefits.
How Have PRP and Stem Cell Therapies Improved Patient Mobility?
PRP and stem cell therapies often produce gradual improvements in pain and mobility by reducing inflammation and supporting tissue repair, with many patients noting progressive gains in walking distance and stair negotiation over weeks to months. For example, a patient with moderate knee OA may report decreased pain on weight-bearing and improved ease climbing stairs by the third month after a combined PRP and rehabilitation protocol. The recovery trajectory typically includes a short period of post-procedure soreness, followed by incremental function gains as inflammation subsides and strength training restores mechanics. Clinicians stress realistic expectations and adherence to rehab to translate biologic changes into durable functional improvement.
These outcomes show the synergy between biologic modulation and mechanical rehabilitation in regaining daily activities.
What Do Patients Say About Life After Avoiding Knee Surgery?
Patients who avoid knee surgery through tailored non-surgical plans frequently describe faster recoveries, less time away from work, and preserved native joint sensation compared with what they anticipated from replacement surgery. Many highlight regained ability to perform specific tasks—walking the dog, returning to low-impact sports, or resuming employment duties—without the extended downtime and restrictions associated with prosthetic implants. Satisfaction tends to correlate with realistic pre-procedure counseling and engagement in prescribed rehabilitation, which help maintain gains over time. These real-world experiences support the value of non-surgical options as viable first-line strategies for appropriately selected patients.
Collectively, success stories underscore the importance of individualized care plans and the measurable outcomes patients can expect when following an integrated non-surgical pathway.
What Are the Most Frequently Asked Questions About Non-Surgical Knee Pain Treatments in Houston?
Patients commonly ask which non-surgical option is best, how long recovery takes, whether insurance covers treatments, and how to schedule an evaluation; concise answers help guide decision-making. Below is a short, practical Q&A table and clear next steps that point readers to scheduling the $49 consultation for a tailored evaluation.
| Question | Short Answer | Where to Learn More |
|---|---|---|
| What is the best non-surgical treatment for knee pain? | The best option is individualized based on OA stage, injury type, and goals; evaluation determines candidacy. | Discuss options during a targeted clinical evaluation. |
| How long is recovery after non-surgical procedures? | Recovery varies: injections/PRP have short downtime; regenerative results often appear over weeks–months. | Recovery timelines are reviewed during planning. |
| Are non-surgical treatments covered by insurance in Houston? | Coverage varies; Campbell Health Center operates independently of insurance and Medicare, so benefits should be checked with your insurer. | Call your insurer and the clinic for specifics. |
| How can I schedule a consultation for knee pain? | Campbell Health Center offers a $49 consultation that includes evaluation and X-rays; scheduling is available by phone or at the clinic address. | Use the clinic phone number or visit the clinic to book. |
Patients should use these concise answers to decide whether to pursue an initial consult and which questions to bring to the appointment. Below are short direct answers to the most common decision-stage questions.
What Is the Best Non-Surgical Treatment for Knee Pain?
There is no single “best” non-surgical treatment for everyone; clinicians select therapies based on cartilage status, pain drivers, patient age, activity goals, and comorbidities to create a tailored plan. For early OA with inflammation, biologic options like PRP may be prioritized; for tendon-driven pain, shockwave and manual therapies can be effective; for vascular-mediated OA pain, GAE may be considered. A focused evaluation, including X-rays and functional assessment, clarifies the most promising path and sets expectations for outcomes. This individualized decision-making model helps patients choose an approach that balances effectiveness, downtime, and long-term goals.
Choosing the right treatment requires diagnostic clarity and a coordinated plan that may combine modalities for best effect.
How Long Is Recovery After Non-Surgical Knee Pain Procedures?
Recovery timelines depend on the chosen therapy: steroid injections often provide quick relief with minimal downtime, PRP and stem cell therapies commonly produce gradual improvement over 6–12 weeks, and GAE patients may notice pain reduction within weeks with short outpatient recovery. Rehabilitation and graded activity are essential after most procedures to reinforce biomechanics and maintain strength, and clinicians provide specific activity guidance to protect healing tissues. Understanding the expected timeline helps patients plan work, caregiving, and activity resumption while adhering to recovery protocols that maximize benefit.
Clear recovery expectations reduce anxiety and improve adherence to rehabilitation plans that support lasting improvement.
Are Non-Surgical Treatments Covered by Insurance in Houston?
Coverage for non-surgical and regenerative procedures varies by insurer; some injections and conservative services may be covered, while many regenerative therapies and advanced procedures commonly fall outside standard Medicare or private insurance benefits. Campbell Health Center operates independently of insurance and Medicare, which allows clinicians to recommend evidence-based options without coverage limitations, but it also means patients should verify coverage and financing options prior to treatment. Calling your insurer and discussing cost considerations with the clinic helps avoid surprises and supports informed decision-making.
Transparent cost conversations during the $49 consultation help patients understand financial implications alongside clinical candidacy.
How Can I Schedule a Consultation for Knee Pain at Campbell Health Center?
To begin, call the clinic at (832) 648-4204 or visit the clinic at 1012 Campbell Rd, Houston, TX 77055 to schedule the $49 consultation, which includes a clinical evaluation and X-rays to determine candidacy and a personalized plan. During the consultation clinicians review symptoms, perform an exam, and review imaging to recommend a staged treatment approach tailored to your goals. Bringing a list of prior treatments and current medications helps speed accurate assessment and decision-making. Booking the consultation starts the three-step process toward a customized non-surgical plan that aims to reduce pain and restore function.
This soft call-to-action provides a clear path to scheduling an evidence-based evaluation and begins the personalized journey to knee pain relief.








